New Delhi: On November 18, the Union health ministry released a letter to reporters. It was written by the health secretary to the chief secretaries of all states and union territories in the country on the same day. The letter asked them to take a series of steps to tackle health issues arising out of rising air pollution levels in Delhi and across India.
On the same day, the Supreme Court came down heavily on the Central Air Quality Management Commission, that consists of officials of Union and state governments, for not doing enough. It also rebuked the Delhi government.
In the letter mentioned above, Union health secretary Punya Salila Srivastava reminded chief secretaries that Atul Goel, director general of health services, who works with the Union health ministry, had written to states on October 19, alerting them about various measures to be taken in the months before the onset of winter – considered to be peak pollution months.
Srivastava’s letter also has the ‘National Programme on Climate Change and Human Health’ (NPCCHH) document enclosed as part of the advisory.
The NPCCHH highlighted a ‘recent’ Indian Council of Medical Research (ICMR) study that has brought out a startling fact – that 17 lakh deaths were ‘attributable’ to ‘air pollution in 2019. This number is significant – a little more than the entire population of Goa. The secretary’s advisory sought to impress upon the state administrators that this was a large number of deaths ‘attributable’ to air pollution every year.
The ICMR and the Public Health Foundation of India (PHFI) conducted the highlighted study in 2019, and its results were released in 2021.
However, the secretary’s letter violates the stand that the Union government has maintained in the parliament and in public statements over the years, wherein it has stated that there is no study which can establish some sort of cause-and-effect relationship between air pollution and deaths.
Although the government has referred to this ICMR study in internal policy documents over the years, it has never mentioned it in public communication.
Sample this answer given by the 2023 Minister of State for Health in parliament on April 6 that year – two years after the ICMR study was published.
“There are several studies conducted by different organisations, using different methodologies, on the impact of air pollution. However, there is no conclusive data available to establish a direct correlation of death/disease/life expectancy exclusively with air pollution. Air pollution is one of the many factors affecting respiratory ailments and associated diseases,” the ministry said.
Many similar replies can be traced to 2023 and the preceding years.
And yet, November 18, 2024, is not the first time that a policy document connected air pollution to deaths.
In fact, the 2022 version of the ‘National Programme on Climate Change and Human Health’, says exactly what the 2024 version says. That, too, went on to detail that chronic obstructive pulmonary disease (COPD), followed by heart disease, stroke and lung cancer attributable to air pollution had led to 17 lakh deaths in 2019.
There was another such ICMR report – a 220-page-long ‘India: Health of the Nation’s States: The India State-Level Disease Burden Initiative’ published with the PHFI in 2017 – which met the same fate.
It said, “Air pollution was the second leading risk factor in India as a whole.”
“Outdoor air pollution caused 6.4% of India’s total Disability Adjusted Life Years (DALYs) in 2016, while household air pollution caused 4.8%. Combined, they make a substantial contribution to India’s burden of cardiovascular diseases, chronic respiratory diseases, and lower respiratory infections.”
DALYs are the years lost to hindrance caused by a particular disease. One DALY represents one year.
This report contained congratulatory messages from the then vice-president of India, Venkaiah Naidu, and the then and current health minister of India, J.P. Nadda, for those who prepared the report.

But the Union health ministry discredited this report in a parliamentary reply on March 23, 2020, saying it was based merely on estimates, without either going into the nuances of the message or its methodology:
“The study report provides the distribution of diseases and risk factors across all states of the country from 1990 to 2016. The five leading risk factors for Disability-Adjusted Life Years (DALYs) in 2016 includes child and maternal malnutrition, air pollution, dietary risks, high systolic blood pressure, and high fasting plasma glucose.
“However, the report is based on estimates as there are no conclusive data available in the country to quantify the extent of mortality/ morbidity, exclusively due to air pollution.”
Nonetheless, the governments before the current National Democratic Alliance government have also shied away from accepting the connection between air pollution and deaths.
In 2007, health minister Anbumani Ramadoss, told the parliament on November 30 that a WHO report claiming that 4.07 lakh premature deaths in India could be linked to air pollution was not sound enough.
He added, “According to a report of Indira Gandhi Institute for Development Research, it is estimated that 4.1 lakh to 5.7 lakh women and young children die prematurely every year due to indoor air pollution caused by burning of biofuels in poorly ventilated homes. However, no conclusive data is available to establish the correlation between mortality and indoor air pollution.”
“No conclusive data” has been the refrain of all governments over at least past two decades.
Lonely battle
Meanwhile, the medical fraternity seems to be fighting a lonely battle alongside the patients. This reporter reached out to a chest physician of a prominent government hospital that caters to thousands of patients everyday on November 18.
When asked as to whether we can link air pollution to death, he replied, exasperated, that everything has been said for the past 10 years has hidden the obvious truth. “The situation is going from bad to worse. Now is the time to ask questions from administrators rather than doctors,” he said.
Dr Arvind Kumar, a prominent chest surgeon and founder of the Lung Care Foundation, has presented a whole range of studies in various meetings organised by the government over the past several years. “I feel saddened and helpless with the response of different policymakers [claiming absence of data], even though they know everything’s there. They act as if they don’t know,” he told The Wire.
Meanwhile, the footfall of patients at healthcare facilities would have gone up as the Air Quality Index clocked at 494 (severe category) on November 18 according to the Central Pollution Control Board bulletin. Many patients who were previously healthy would now need treatment, say doctors.
It is not possible for any clinic or hospital to quantify the surge at out-patient respiratory departments accurately because such record-keeping is not done. There are hardly any dedicated air pollution clinics in the city.
“Moreover, the full effect would only be felt in the next two to three days,” Dr Sreedev Narayanan, a resident doctor at the respiratory medicine department of a city-based private hospital said on November 18.
However, recounting his experience of the last five years, Narayanan said that the number of patients who get admitted or even who land in emergency departments go up as the air quality worsens. These are people with pre-existing respiratory problems like asthma or tuberculosis.
“The pollutants can cause bronchus to collapse almost completely in patients who have pre-existing respiratory problems,” Narayanan said.
The load in the in-patient departments where admission takes place doubles or triples during this two or three-week duration every year. This is especially true, again, for patients with pre-existing illnesses. “Their threshold of tolerance is very low,” said Dr Anmol Jindal, a resident doctor associated with the department of internal medicine of a city-based private hospital.
Jindal explains that exposure to pollution may lead to swelling in lungs of patients who are already unhealthy. This may make it difficult for them to exhale carbon dioxide, causing death.
“We have to resort to steroids [for patients], who had been otherwise responding well to prescribed medicines before onset of ‘pollution months’. They would not have needed steroids had the pollutants not aggravated their illness, ” he said.
Besides these bits of empirical evidence, there exists year-wise and cause-wise data that the WHO has maintained for all countries, including India, on air pollution and deaths. According to it, 8.9 lakh deaths took place in India in 2019 alone due to diseases linked with air pollution. This is quite conservative a number as compared with 17 lakh deaths that the ICMR-PHFI study estimated for 2019.
The WHO figures were based on the secondary data sources while the researchers for the ICMR-PHFI study collected first-hand information. They adopted a robust methodology by using aerosol optical depth data from multiple satellite sources combined with a chemical transport model. This data was calibrated with data from ground-level monitoring station locations in India
From 2010-2018, 3-8 lakh deaths took place each year because of this annual killer, according to the WHO. The year-wise data sets can be found below:
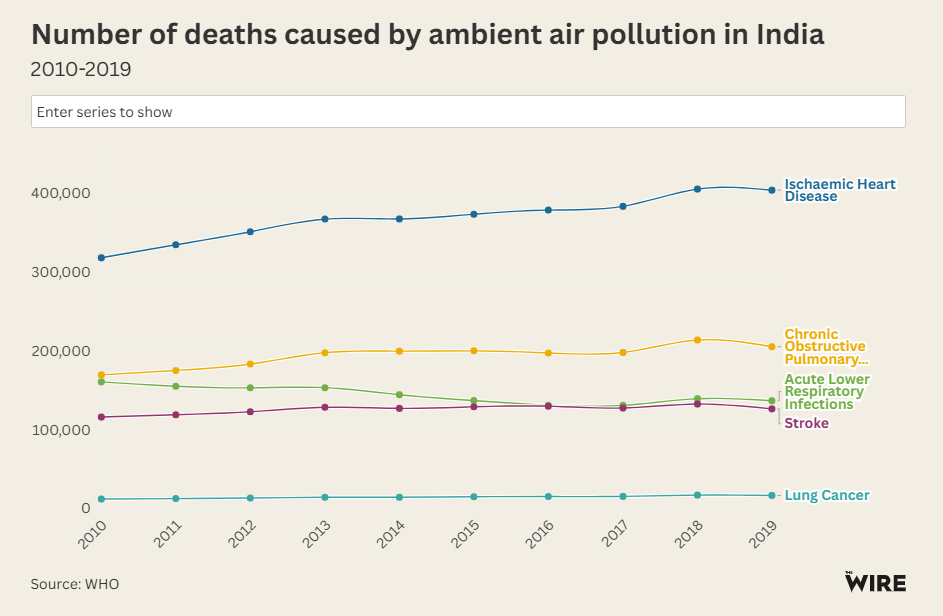
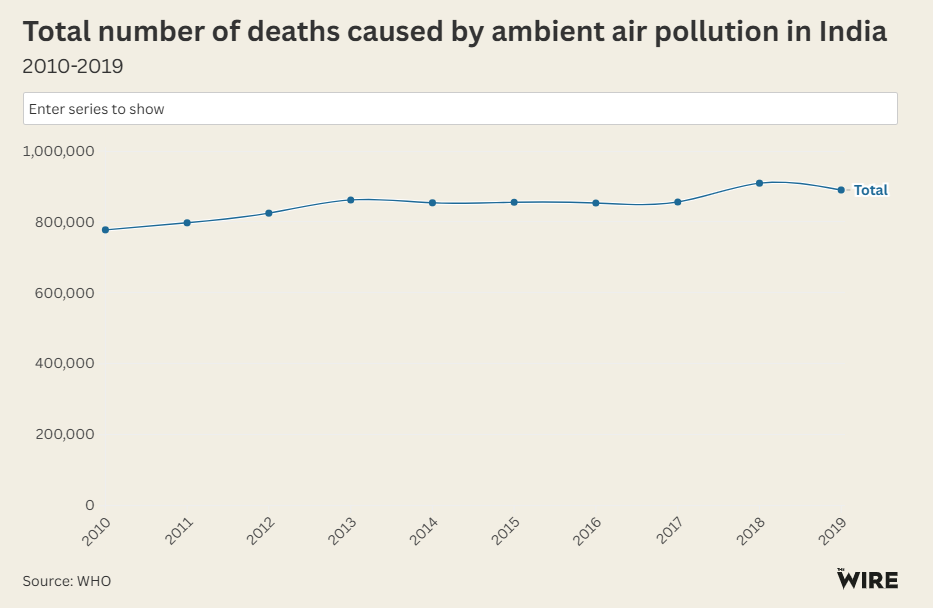
In nutshell, air pollution paves the way for all these five major life-threatening diseases, invisibly causing a slow death. However, the government has been rejecting this data as inconclusive.
Besides causing these big five diseases mentioned in the WHO database, air pollution has been linked with skin problems, ophthalmological issues, mental health disorders, dementia, stillbirths, anaemia, decreased fertility rates, and host of other illnesses affecting the nearly whole body.
Children, meanwhile, are the worst sufferers. A foetus gets exposed to air pollution through its mother. Kumar, quoted above, says, that given the situation in Delhi now, within the first hour of birth, a child is born with lungs that are the equivalent of them having smoked a few cigarettes.
Exposure to pollution can lead to brain inflammation of mild levels in children. This can make them hyperactive. They may cause an attention deficit. Their lung development may be hit at a tender age. Their IQ development is impacted. The arteries and pancreas get affected too – Kumar goes on.
“Some of these can really have long term impacts, even beyond teenage. Nowadays I am not surprised to see black spots in the lungs of teenagers who are non-smokers,” he adds.
Meanwhile, the ban on crackers continues to be flouted in many parts of Delhi, even now. Dr Parth Sharma, a community health physician and a public health researcher, says ongoing studies in Delhi have shown a higher degree of presence of heavy metals in the blood of people, two days post-Diwali as compared to the pre-Diwali days.
Heavy metals like copper, arsenic, zinc, cadmium and selenium are found in crackers. Exposure to these heavy metals, over years, can cause endocrine (hormone) disorders and cancer.
Both Kumar and Sharma highlight that not only do morbidity and mortality increase due to air pollution, but so does the financial burden.
“The average cost of one asthma pump is Rs 300-400. In government hospitals, it is mostly out of stock – how are poor people going to afford it?” Sharma wonders. Kumar says he has seen exponential increase in sales of nebulisers for children, along with cough syrups and inhalers.
The sale of air-purifiers also shoots north. But the doctors caution that they may not work as well as imagined by people. Every air purifier has a handling capacity, and it has to be installed according to the volume of the room. A small purifier in a big room is of no advantage – besides being the least affordable alternative.
Insofar as masks are concerned, cloth or surgical or any other types of masks do not work outdoors to filter PM 2.5 (particulate matter Smaller than 2.5 microns; one micron being one millionth of a metre). The government advisory, as doctors also say, notes that only N95 or N99 masks can work. These are currently being sold at several times their original cost.
Neither the Union nor the Delhi state government have taken any steps to provide these masks at subsidised prices or to try to curb the abnormal price rise. No government has shown any urgency in creating awareness about masks either. These are small but effective initiatives. Yet they have, so far, not figured in plans of any government to mitigate the effects of pollution on health.
(This article was first published in The Wire)
Also Read: Anmol Bishnoi, Brother of Jailed Lawrence Bishnoi, Detained in US